Grand Rapids Red Project Works to Stop Overdose Deaths

Julie Bitely
| 5 min read

Unless it’s a high-profile actor or musician, overdose deaths don’t typically get a lot of attention. However, the problem is bigger than you think.
In fact, Michigan is one of many states to recently pass legislation that expands access to the overdose-reversing drug, naloxone.
For a small, grassroots non-profit organization in Grand Rapids, getting naloxone in the hands of those at risk for overdose has been part of a larger mission for the past six years.
The Grand Rapids Red Project formed in 1998 as an organization dedicated to preventing the spread of HIV. In 2000, the mission expanded to include a syringe exchange program, CleanWorks, which now also encompasses a comprehensive harm reduction program. Syringe exchange clients started receiving naloxone prescriptions and training to successfully administer the drug starting in 2008.
The prescription drug can be injected or administered nasally to reverse an overdose from heroin or prescription opioid painkillers. Red Project works with two local doctors to prescribe the injectable form of naloxone to existing clients and their family and friends.
Since the program started, almost 1,000 people have been trained to administer naloxone and 185 overdose reversals have been reported.
A Big Problem with a Known Solution
Overdose is the leading cause of accidental death for people ages 21-65 in Kent County. Deaths in the United States from prescription opioids have risen steadily, with 16,651 deaths attributed to the drugs in 2010, the most recent year data was available from the Centers for Disease Control and Prevention.
“More people are dying on a daily basis in Michigan from drug overdose than they are from car accidents,” said Dr. Sandy Dettmann, an addiction medicine specialist, who prescribes naloxone to Red Project clients.
Being able to administer the drug quickly buys valuable time when people are waiting for medical personnel to arrive. Dettmann knows firsthand how important timely delivery of the drug can be. She was chronically ill and on multiple prescription medications, including powerful opioids– medications to either help her get better or to allow her to die in peace. Her personal story illustrates that you don’t have to be a drug addict to overdose on opioid medications.
“Naloxone saved my life and I believe that my life was worth saving,” she said. “I was on multiple medications and didn’t know what I was doing. When a person’s ability to think rationally is compromised by medications, accidents happen. That’s why we prepare for them by having life-saving antidotes available.”
Dettmann and Red Project Executive Director Steve Alsum both liken those at risk for overdose with bee sting allergy sufferers. Just as the latter group wouldn’t leave the house without an epi-pen, those using prescribed or non-prescription opioid drugs should have a rescue kit that includes naloxone.
“It’s a tool that could potentially save their lives,” Alsum said. “Hopefully, they’ll never have to use it.”
Meeting People Where They’re At

A mobile unit helps the Grand Rapids Red Project deliver services to people in their own neighborhoods to overcome issues of access.
People who utilize the harm reduction services of the Grand Rapids Red Project are all at different places in their lives. Staff members and volunteers don’t push an agenda of recovery, rather, they offer a refuge of understanding. Alsum explains that many staffers and volunteers have histories of drug use themselves and try to meet clients where they are, with no judgment.
“A lot of times, the best person to reach someone using drugs is someone with a similar experience,” Alsum said. “Our clients really appreciate that aspect of our program.”
He said that drug use happens in every community and that nobody deserves to die because of a mistake. By keeping drug users healthy through the syringe exchange program and alive through naloxone distribution and training, clients are free to chart their own future.
“Nobody will deny that drug use can be an extremely harmful and dangerous behavior,” Alsum said. “Not everybody is ready to get clean today and not everybody has the support systems around them to be successful today.”
Making the choice to use clean syringes or receive naloxone training is a healthy step that can lead to bigger changes down the road.
“Somebody will start making small changes and will be successful in making those small changes, and throughout that process they’ll start to make bigger changes,” Alsum said.
From Client to Counselor
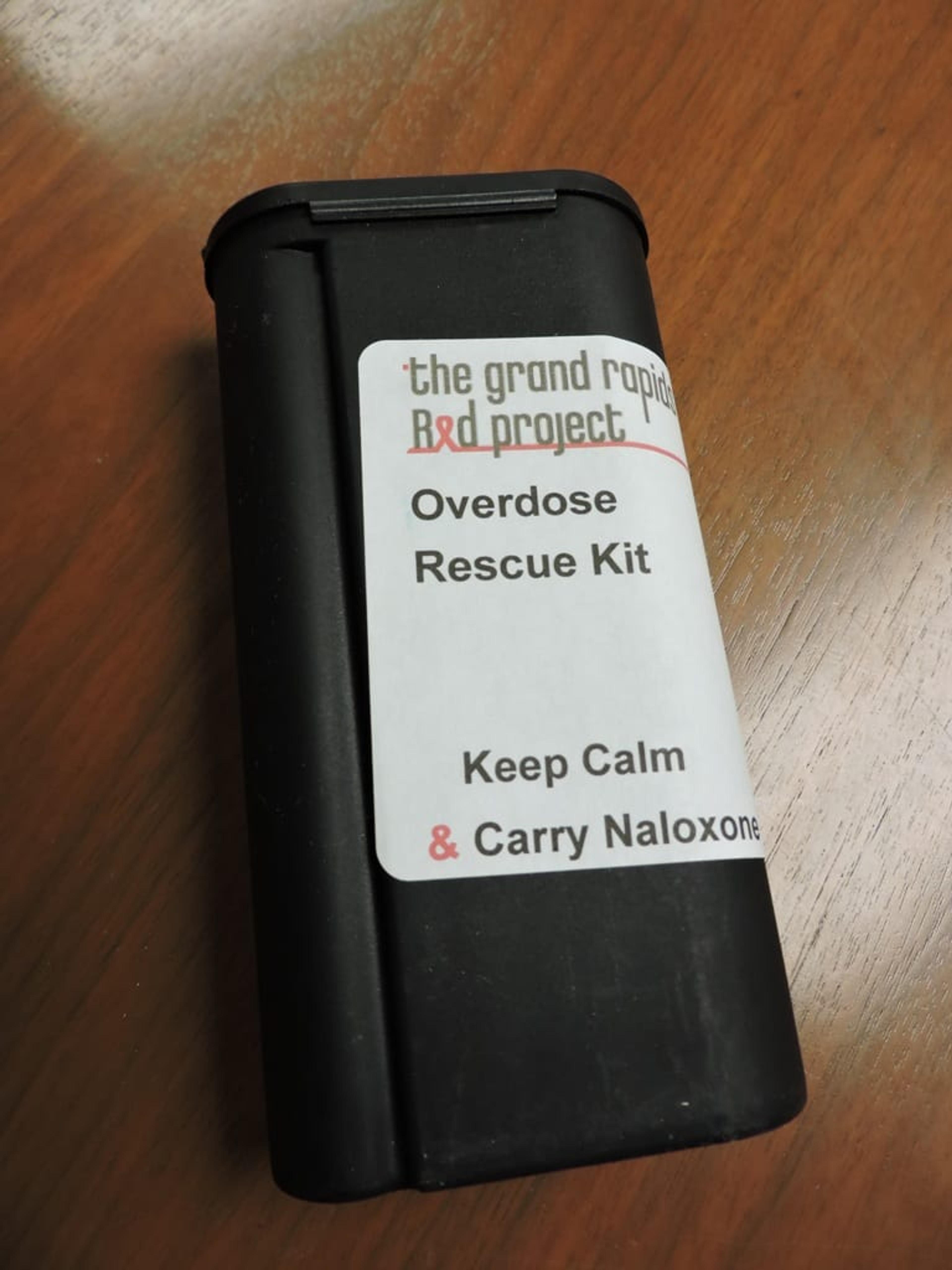
A naloxone recovery kit distributed by the Grand Rapids Red Project.
It took Brandon Hool many stops and starts before he kicked heroin.
A downward spiral into drugs started with using alcohol and other substances at a young age to cope with feelings of social awkwardness. Hool remembers thinking the drug education he received in school was wrong.
“Nothing bad happened right away like they said it would. Better stuff started happening,” he said of his new found social ease and acceptance at school.
Still, it was never enough and the years following high school passed by in a haze of rehab and stints in jail and prison. He also contracted Hepatitis C and kept having friends overdose and die.
“That could have easily been me,” he said.
Eventually a supportive recovery community helped Hool find the personal connection he thought drugs and alcohol would supply. After a successful rehab stint in 2010 he started volunteering with Red Project and hasn’t looked back.
“That’s what I was missing when I started, that connection,” he said. “I got into the recovery community and I was part of something.”
Now, Hool works as Red Project’s Clean Works Program Manager. He said working with the group as a volunteer and staff member are a huge part of his continued recovery. He’s had clients come in and tell him they saved a life or had their life saved.
He only wishes the friends he lost to drug use would have had naloxone as an option.
“They didn’t have that,” he said.
For more information on the Grand Rapids Red Project, visit redproject.org.
Photo credit: Katie Mollon





